Abstract
Background: Sickle cell disease (SCD) is an inherited condition affecting over 100,000 individuals in the United States with increasing prevalence, with annual healthcare costs of approximately $488 million dollars. Peak rates of healthcare utilization occur in the young adult population, with the highest mortality risk when transitioning to adult care. This has prompted increased efforts to improve the transition process from pediatric to adult care, in addition to optimizing overall care for SCD patients. The impact of these efforts on current healthcare utilization, including reasons for hospitalization, has yet to be explored. This study sought to explore current rates of healthcare utilization in SCD patients, measured by inpatient hospitalizations, as well as the most common reasons for hospitalization to inform continued efforts to improve outcomes in the SCD population.
Methods: Data was obtained from the Healthcare Cost Utilization Project (HCUP) State Inpatient Database (SID) for New York from 2005-2014. All patients with a principal or secondary ICD-9-CM diagnosis of any genotype of SCD (282.41, 282.42, 282.60-282.64, 282.68 or 282.69) were identified. Patients with anemia or other hemoglobinopathies not due to sickle cell were excluded. The encrypted identifier was used to identify all hospitalizations in SCD patients (including those not coded for SCD), and analyze outcomes at a patient-level. Utilization outcomes examined were (1) total number of patient encounters and (2) 30-day and (3) 90-day readmissions following the index hospitalization. To examine reasons for hospitalization, variables for common conditions were created using standard ICD-9-CM diagnosis codes found in the Elixhauser Comorbidity algorithm, a tool used to predict hospital resource use and in-hospital mortality, in addition to acute or chronic conditions associated with SCD. Descriptive statistics and univariate analyses were performed using SAS Enterprise Guide version 7.1. This project was determined to be exempt from Institutional Review Board oversight per the Washington University Human Research Protection Office.
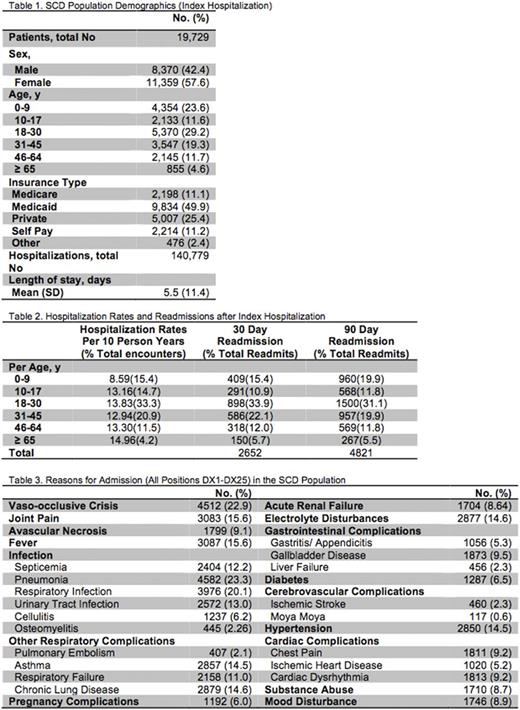
Results: A total of 19,729 patients had at least one hospitalization from 2005-2014 coded for SCD, with a total of 140,779 hospitalizations. The SCD population was 57.6% female and the primary insurance type was Medicaid (49.9%). The mean age at index hospitalization was 26.5 years (SD 19.3, range 0-104) and the mean length of stay was 5.5 days (SD 11.4). At the time of the index hospitalization SCD patients aged18-30 years made up 29% of the population (Table 1). The largest percentage of all hospitalizations also occurred among patients in this age group (33.3% of total encounters). Hospitalization rates per 10 person-years of observation were similar among patients aged 10-17 years (13.2), 18-30 years (13.8), 31-45 years (12.9) and 46-64 years (13.3). Both 30-day and 90-day readmissions after the index hospitalization were highest in the 18-30 year age group (33.9% and 31.1%, respectively, Table 2). The most commonly coded diagnoses were pneumonia (23.3%), vaso-occlusive crisis (22.9%) and respiratory infection (20.1%, Table 3). The most commonly coded principal diagnosis was vaso-occlusive crisis (11.7%). Diagnoses associated with the respiratory system accounted for the largest category of hospitalization reasons, including: pneumonia (23.3%), respiratory infection (20.1%), asthma (14.5%), respiratory failure (11.0%) and chronic lung disease (14.6%). (Table 3)
Conclusion: Analysis of 10 years of inpatient data shows that overall rates of hospitalizations in SCD patients have decreased as compared to those previously reported in the literature. Rates per person years were similar across most age groups, but 30-day readmission, a frequently used quality metric, was highest in the young adult age group. This suggests an improvement in utilization patterns, but also reiterates the need for targeted efforts towards improved care in the young adult group. Hospitalizations were frequently due to vaso-occlusive episodes, and a large number of hospitalizations were due to complications of the pulmonary system, both infectious and non-infectious. Directed efforts towards optimizing pulmonary health and aggressive treatment of respiratory infections may further decrease the utilization burden and hasten the improvement of outcomes in the SCD population.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal